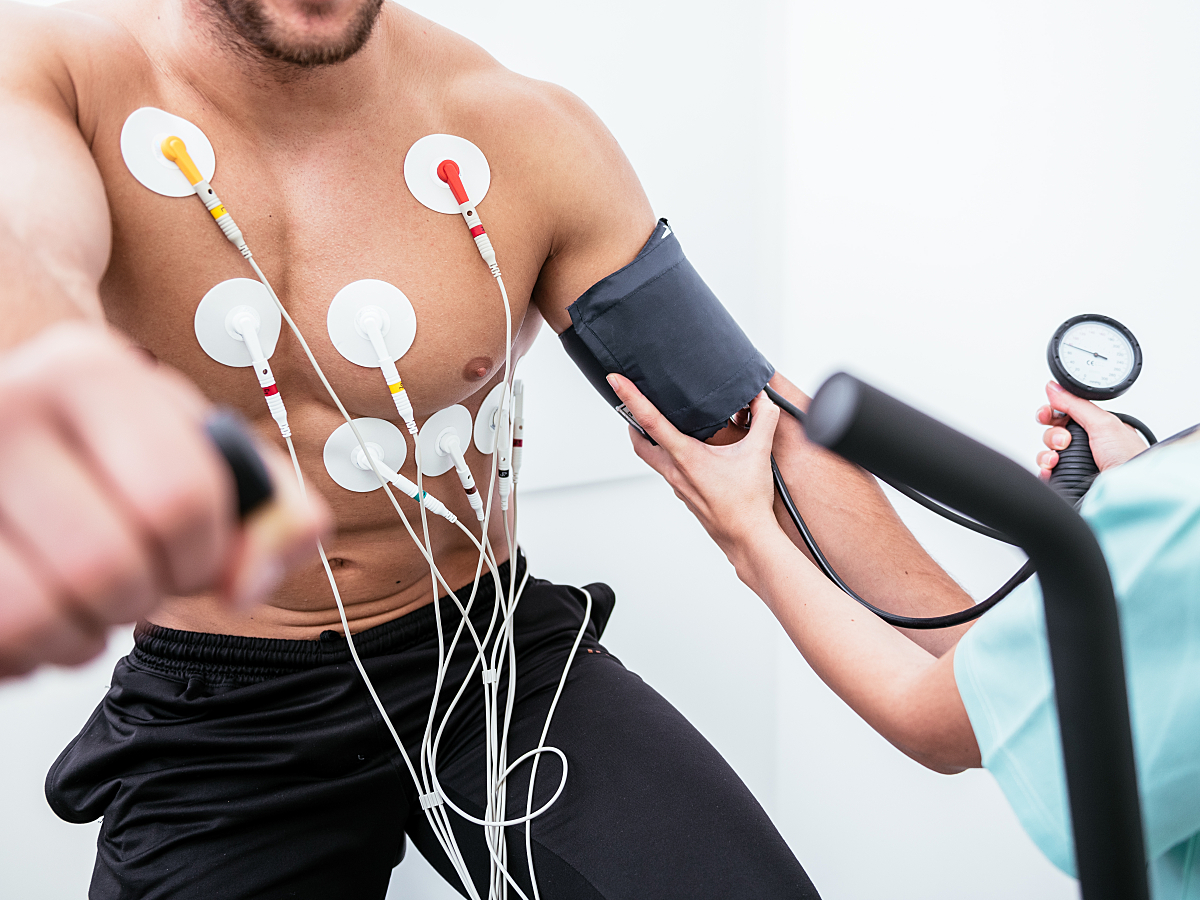
Many variables are considered when interpreting a stress test, not the least of which are the ST segment response and other waveform readings. Yet, in addition to ECG interpretations, abnormalities in blood pressure response during exercise can also be one of the most telling assessments in the context of exercise stress interpretation.
Unusual patterns of blood pressure activity—or elevated peaks during increased physical activity—can indicate an underlying concern relative to the patient's health and cardiovascular risk profile, such as the narrowing of the arteries. In addition, understanding the relationship between blood pressure and other variables such as heart rate during exercise—a measure known as the Double Product—can further inform workups and treatment planning.1
Given the literature indicating the importance of these additional variables when interpreting exercise testing, manufacturers have developed integrative equipment and algorithms to facilitate such assessments. This means it may be easier than ever to collect and contextualize accurate and reproducible multivariable stress testing data for a more comprehensive cardiovascular picture.
Here's what clinicians should know about the why and how when examining blood pressure response during exercise.
Blood Pressure Response During Exercise: What's Normal, What's Not
During exercise, healthy individuals experience a maximum blood pressure of up to 250 mmHg. Moreover, stress-induced diastolic blood pressure should only increase by up to 10 mmHg. Anything above these thresholds is considered abnormal and may warrant further assessment to monitor for health concerns, such as coronary disease.1
In addition to this absolute maximum number, certain patterns of blood pressure changes in response to exercise may be considered normal or abnormal depending on the stage of exercise—maximal (peak) or submaximal (non-peak)—the patient is experiencing.
Normal blood pressure:
- Raises first when starting exercise.
- Potentially but not always drops at peak effort.
- Rises again after the activity ends.
- Goes back down during recovery.
Throughout exercise, the increase should not be too pronounced and align with the expected blood pressure ranges for adults already noted.
One 1970s-era study assessing healthy participants observed a delta of 61 ±19 mmHG in men and 42 ±18 mmHG in women, as one reference point.1 If those being tested demonstrate patterns that deviate from this—particularly if blood pressure drops before maximal or submaximal effort—it may be considered abnormal.
The Role of the Double Product of Blood Pressure + Heart Rate
The Double Product, also known as the rate pressure product (RPP), is a combined measure of the heart rate and systolic blood pressure. By considering these two assessments individually and in conjunction with one another, clinicians get the benefit of understanding heart function and myocardial oxygen demand.
In healthy individuals, heart rate increases with more effort before plateauing at peak or near-peak levels. The authors of a study in The American Journal of Cardiology, assessing healthy participants, observed a change of 108 ±14 beats per minute in men and 94 ±15 beats per minute in women, for example.1
Maximum RPP can be quantified by multiplying heart rate and systolic blood pressure together at minute intervals throughout the duration of the exercise evaluation and identifying the top value.2 In healthy individuals, RPP will be higher than 20,000 mmHg per minute. If that normal threshold exceeds the actual maximum RPP, it may indicate concerns relative to myocardial oxygen demand and necessitate further examination. Anything below 16,000 mmHG per minute is considered an insufficient rate pressure response.1
Risks to Watch for When Considering Stress-Related Blood Pressure
One of the many benefits of evaluating blood pressure response during exercise is to assess for stress-induced concerns such as abnormally elevated blood pressure during and after physical activity. Such measures could help predict heart disease and even death. The well-known Framingham Heart Study identified such a relationship among its 1,993 "midlife" participants (at the average age of 58.)3
These rises may even occur in hypertensive patients who otherwise have their blood pressure under control with medications. One study found that many such patients who took hypertensive medication saw pronounced increases in their blood pressure when they reached just half of peak effort. Interestingly, while more study is needed, the author of that study encouraged clinicians to consider medication-resistant exercise peaks when determining maintenance plans.4
Similarly, hypotension can also be identified through stress blood pressure testing as a known predictor for arterial narrowing, especially double- or triple-vessel disease. One study found that 6 of 96 patients with double-vessel disease and 15 of 88 with triple-vessel disease experienced hypotension during exercise.1
When combined with other measures such as heart rate, additional considerations may materialize. An insufficient RPP, as one common example, has prognostic value for future cardiac events, perhaps even more accurately than age-predicted maximum heart rate or the heart rate reserve.2
Cardiologists may want to consider these results in conjunction with further testing, such as coronary angiography.
Stay on top of cardiology trends and best practices by browsing our Diagnostic ECG Clinical Insights Center.
Equipment and Configurations for a Seamless Test Experience
With the value of blood pressure monitoring apparent during ECG testing, many manufacturers have made efforts to better connect multiple assessment technologies for a more seamless clinician and patient experience.
A dedicated integrated exercise blood pressure device can help acquire blood pressure measurements consistently and reproducibly at defined points in the exercise protocol, allowing the operator to focus on the patient and eliminate the variations introduced via manual measurement.
Optimizing the Data Possibilities of Exercise Testing
Although ECG interpretations can serve as a powerful indicator of heart function and inform potential interventions, cardiovascular health is multidimensional and complex—so requiring comprehensive evaluation, too. Many different variables can factor into workups and care pathways, including blood pressure and heart rate. These two insights are essential as they can help contextualize and inform care planning for several conditions, from identifying narrowed arteries to assessing myocardial oxygen demand.
When clinicians can approach exercise tests from a more efficient and connected standpoint that accounts for these diverse variables, they get the benefit of increased assessments and metrics that might not otherwise be available. And patients, of course, potentially get a more satisfactory testing experience.
Fortunately, testing equipment has evolved to meet these nuanced needs, not just with systemic programming to support diagnostic decision-making but also with more integrated toolsets for easier examinations across blood pressure and beyond. These resources help to deliver more comprehensive workups for every patient—and with them, more comprehensive care pathways, as well.
Resources:
1. Irving JB, Bruce RA, DeRouen TA: Variations in and significance of systolic pressure during maximal exercise (treadmill) testing. The American Journal of Cardiology. 1977; 39(6):841-848. https://doi.org/10.1016/S0002-9149(77)80037-4.
2. Whitman M, Jenkins C. Rate pressure product, age predicted maximum heart rate or heart rate reserve. Which one better predicts cardiovascular events following exercise or echocardiography? American Journal of Cardiovascular Disease. 2021;11(4):450-457. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8449196/.
3. Lee J, Vasan RS, Xanthakis V. Association of blood pressure responses to submaximal exercise in midlife with the incidence of cardiovascular outcomes and all‐causemortality: The Framingham Heart Study. Journal of the American Heart Association. 2020;9(11). https://doi.org/10.1161/JAHA.119.015554.
4. American Heart Association. Medicine fails to control blood pressure during exercise. heart.org. https://www.heart.org/en/news/2018/07/11/medicine-fails-to-control-blood-pressure-during-exercise. Accessed December 1, 2022.