There are around 620 million people across the world living with heart disease and that number is on the rise.
Given this prevalence and the increased incidence, it’s critical that the way in which we diagnose and treat heart disease continues to evolve.
Interventional cardiology specifically, and the tools that these physicians use, have evolved and are continuing to do so. This is especially true of stents and procedures such as Percutaneous Coronary Intervention (PCI) that are performed countless times per year around the globe.
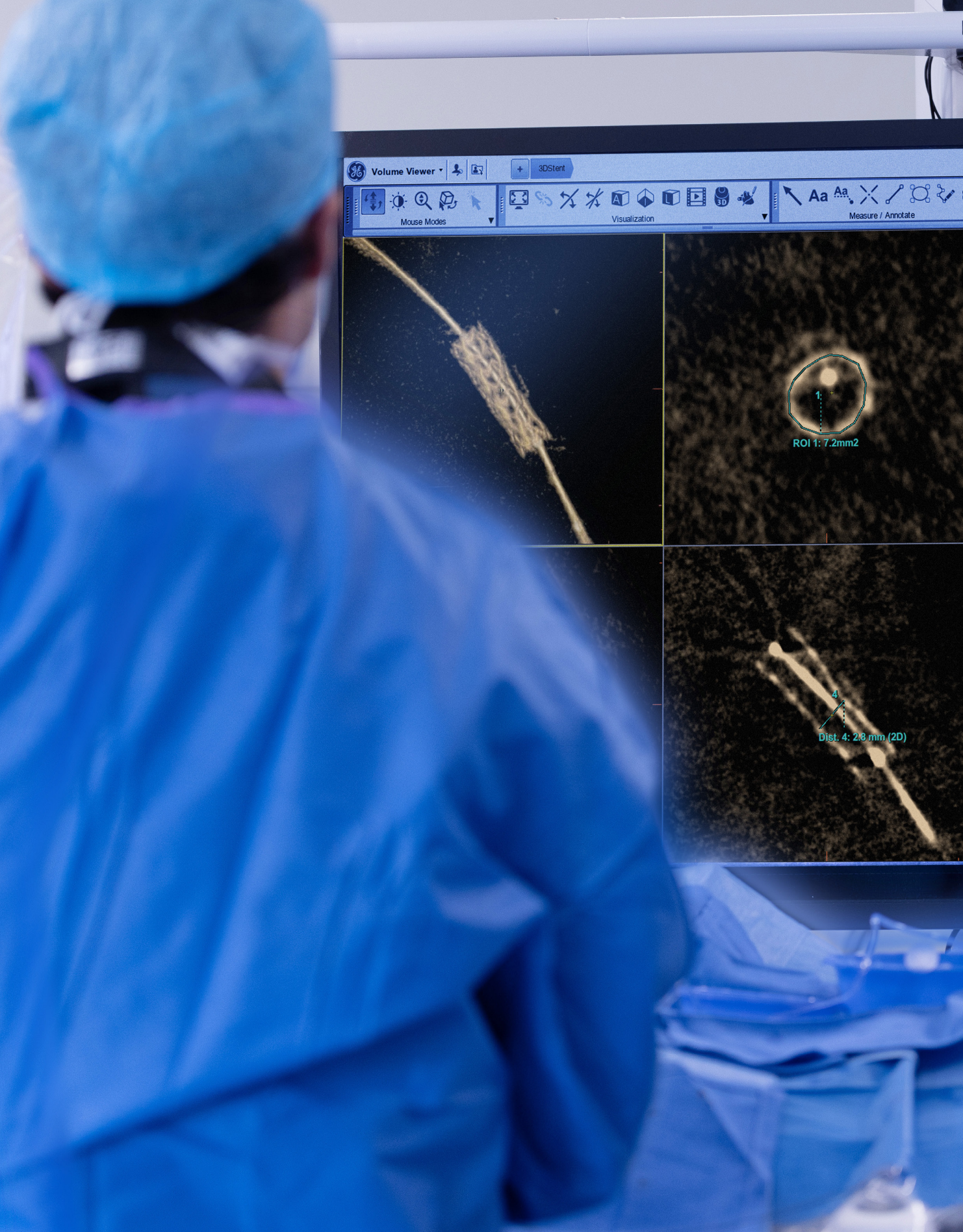
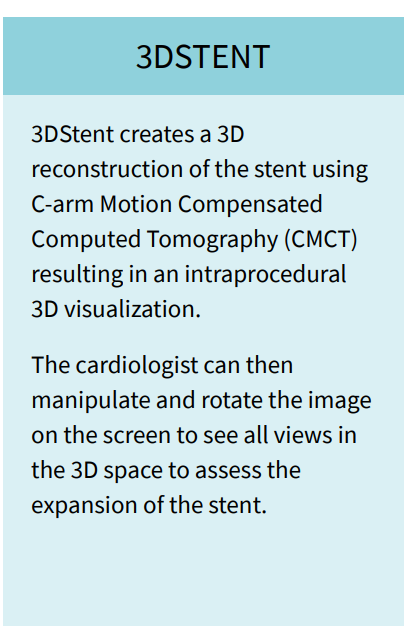
Now, clinicians will have a new tool to use in the Cath lab to help provide clarity and important information during procedures. 3DStent from GE HealthCare will, for the first time, allow clinicians to visualize the stent in 3D using only rotational angiography, without any additional device.
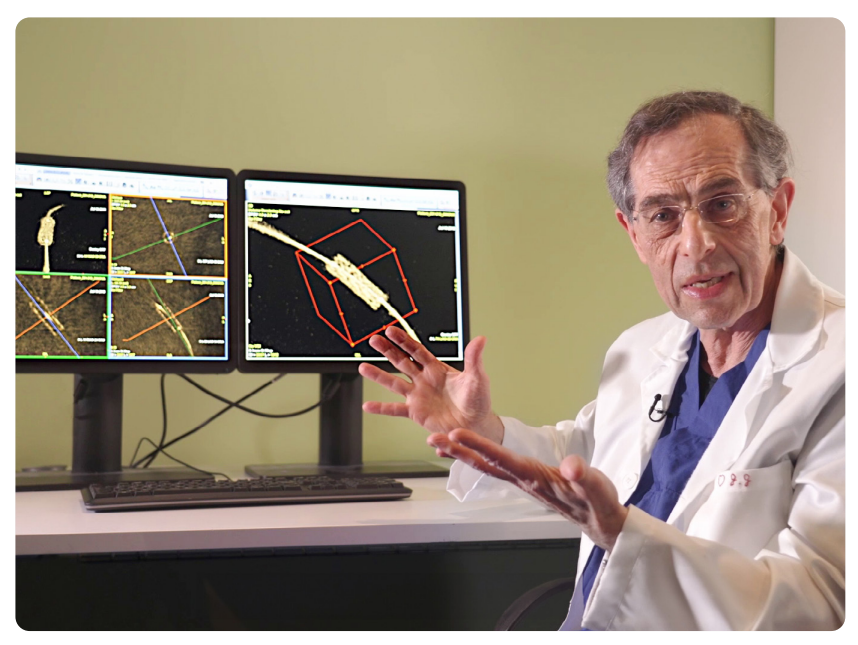
We had the opportunity to talk with three leading interventional cardiologists about the challenges they face, advances in technology and the future of PCI.
We started by asking each physician to tell us a bit about their practice.
Dr. Benamer : I am an interventional cardiologist working in different centers around the Paris area, performing Percutaneous Coronary Interventions as well as structural heart procedures such as TAVI, Patent Foramen Oval closure and a few left atrial appendage closures. We see all types of patients both chronic and unstable, and I am performing more than 500 angioplasties per year.
Dr. Collet : I’m an interventional cardiologist at the Cardiovascular Center Aalst in Belgium. Every day, my job consists of doing diagnostic and therapeutic interventions in coronary arteries. We are a Cath lab treating approximately 1,000 coronary patients a year and we treat all types of coronary artery disease including the challenging calficic disease. In the Cath lab today we receive a mix of about 50% of the patients with stable coronary artery disease and the other 50% of the patients come to us with an acute coronary syndrome.
Dr. Guagliumi : Galeazzi Sant’Ambrogio is a new hospital that recently opened its doors in the innovation district in Milan. It is a fusion of the experience of many years accumulated by the doctors at the Sant’Ambrogio with a passion for innovation. It spans the entire spectrum of interventional cardiology including coronary artery disease, especially highly complex disease. We do a lot of imaging and handle about 1,000 coronary artery interventions per year.
What are the challenges you are facing during PCI procedures, especially when stenting lesions?
Dr. Benamer : The different issues we face with coronary angioplasty are twofold. The first challenge is the setup of the stent for which we can use different tools to help approach calcified lesions and prepare the vessel. Then, once the stent is placed, we must ensure that it is correctly expanded since that has an important impact on the patient’s long-term prognosis.
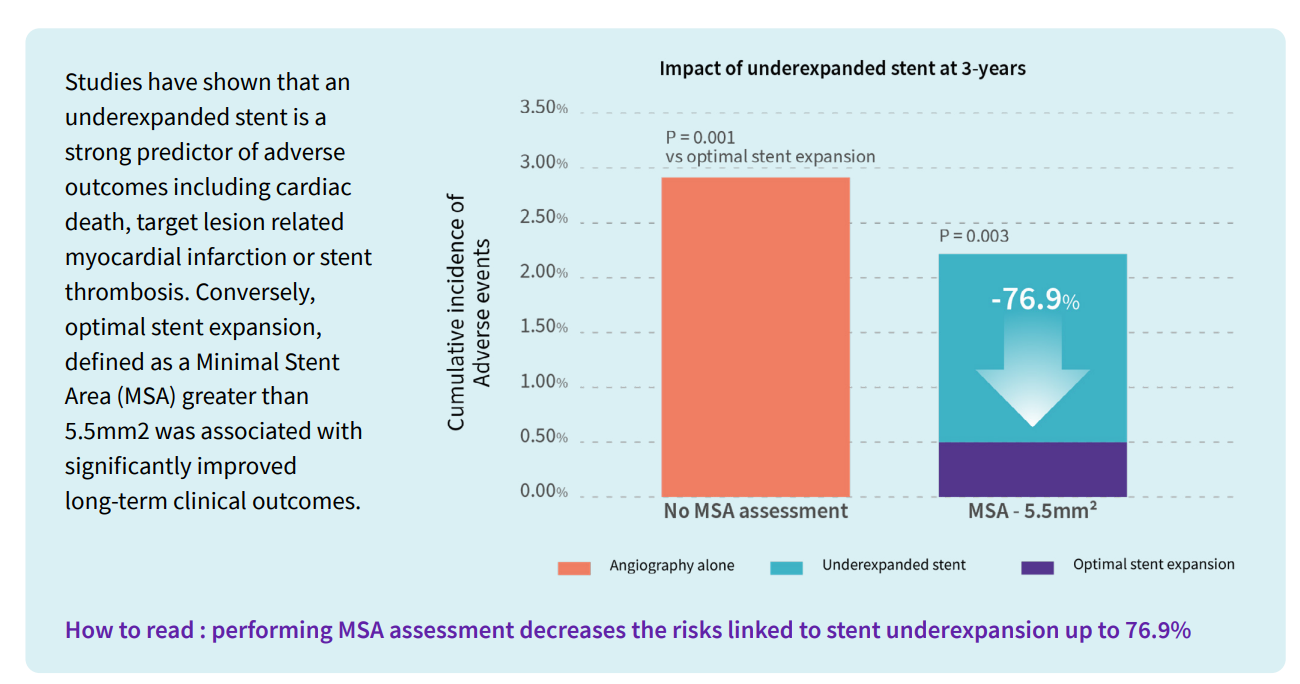
Dr. Collet : Calcium is an important element in predicting stent under expansion. If you are unaware of the plaque that you are treating and you implant the stent in a heavy calcific lesion, the minimal stent area will remain low, and we have seen how Important that is in terms of outcomes.
Dr. Guagliumi : The challenges we are facing with coronary interventions are more or less spreading across the entire world and it’s driven by the increasing complexity of the patients due to factors like age and comorbidities such as diabetes and renal failure which means more calcium. So, it’s a more difficult procedure and more demanding in terms of achieving optimal results.
Can you explain the risk of stent under expansion and the reasons behind it?
Dr. Benamer : We know today that under expansion of the stent impacts long term outcomes for the patient and can increase mortality by leading to complications such as thrombosis. Additionally, incorrect deployment of the stent, including stent under expansion, can elevate the risk of restenosis of the targeted vessel.
Dr. Collet : When we implant the stent, it is very important that the stent is well expanded. Why? Because under expansion - and that can be expansion rate under 80% or simply a small stent area - is associated with something that we call target vessel failure. What is target vessel failure? A combination of death, myocardial infarction and stent restenosis. So, patients that have stent under expansion have a higher risk of stent restenosis and stent thrombosis.
Dr. Guagliumi : One of the biggest challenges in these highly complex cases is in to get a full expansion of the stent and doing it carefully and getting the measurements and the visualization of what we are doing. When you are expanding the stent, many times you stay under expanded and the main reason behind that is calcium. Calcium is the most important enemy of stent expansion.
How are clinicians currently assessing stent expansion?
Dr. Benamer : I am a strong believer and a strong user of StentViz but when we only have an image in 2D we can lose some information about the stent’s expansion. When needed, we have the capability to use intravascular imaging tools to confirm the correct expansion of the stent and assess peripheral under expansion of the stent.
Dr. Collet : Over the past few years, the field of intracoronary imaging has really provided us with novel insights and is allowing us to improve the work that we’re doing by understanding how we implant the stent and importantly how the stent was expanded after the procedure. Additionally, there are ways to assess stent expansion that leverage the techniques coming from angiography that actually enhance the stent image after implantation. Today, these are widely available from several of the vendors. For example, you have the technology like StentViz from GE HealthCare and there are others from different OEMs.
Dr. Guagliumi : Assessing stent expansion is becoming more and more important. How are we doing? Well, for the vast majority of the interventional cardiologist, angiography remains the referral point. But we know that angiography has a clear limit in getting the details of the stents. This was the reason behind the increase in enhanced technology in angio to try to detect the border of the stents.
Why would you need intravascular imaging during PCI procedures?
Dr. Benamer : There is a general agreement around the value of intravascular imaging to get the most possible information about the stent and its expansion – especially if there is any doubt. Unfortunately, the proportion of cases using intravascular imaging is still low - less than 10% France - but for risky angioplasty the clinician must leave no doubt as to the result. (from the Sympo)
Dr. Collet : There are a number of trials in the field of intravascular imaging that will likely demonstrate that assessing the extent of stent expansion with intravascular imaging results in better outcomes compared to angiography alone.
Dr. Guagliumi : There is a growing attention toward intravascular imaging as it is able to navigate inside and make precise measurements. Of course, these are additional technologies with additional costs. And you need additional training, though artificial intelligence is helping make intravascular ultrasound and OCT easier. On a global scale, intravascular imaging is strongly underused, and many say that it’s too complex. There are regions like Japan where intravascular imaging is used in more than 90% of the cases with the great results. There is a longer tradition there. In the US it goes down into 15% and in Europe it goes down to 5-8%. That is too few to guarantee a high level of precision in what we are doing with the stents.
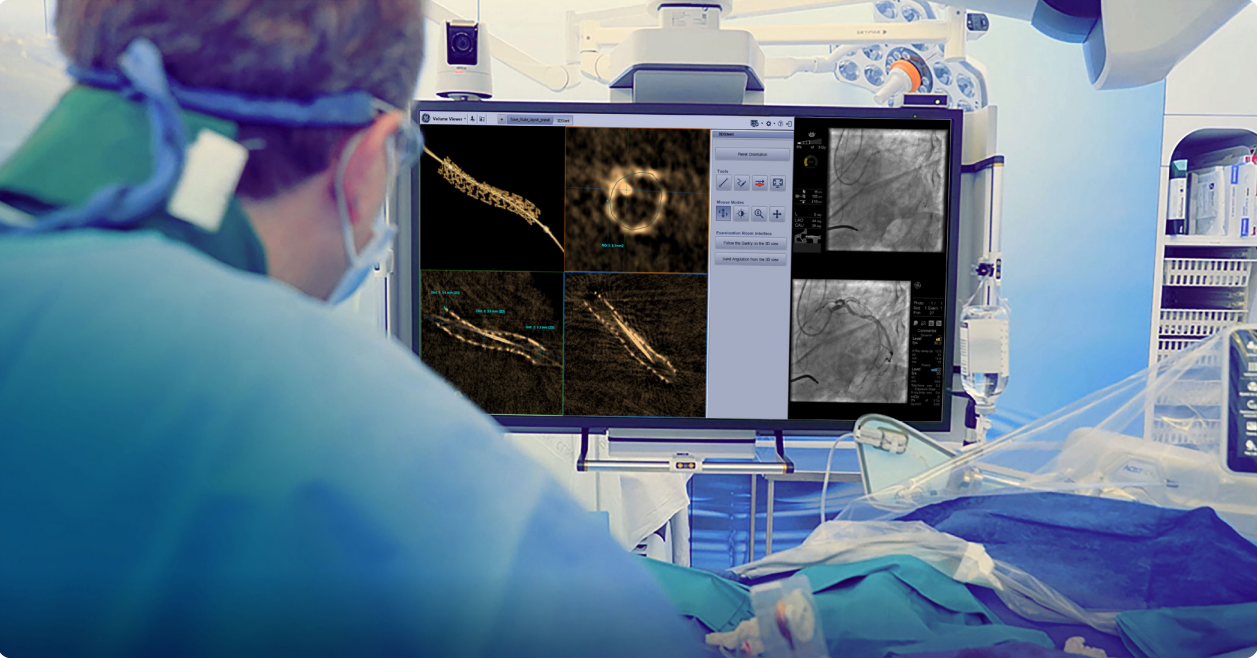
GE HealthCare’s new 3DStent uses C-arm Motion Compensated CT (CMCT) to provide three dimensional images of the stent during the procedure. Can you tell us what potential you see in this innovation ?
Dr. Benamer : This will allow a good visualization of the stent over the three dimensions. We can assess stent under expansion but also the root cause of an under expansion over the different slices displayed on the large display monitor. The acquisition is easy and doesn’t require any additional device or contrast injection making it a complement to our current tools of visualization.
Dr. Collet : This new technology lets us assess stent expansion using angiography and is actually using existing concepts like stent enhancement and mixing that with rotational angiography. The result is a three-dimensional depiction of the stent done inside the Cath lab during the PCI. This is the first time we can quantify MSA only with angiography and, for me, this is one of the biggest steps forward.
Dr. Guagliumi : We know it’s important to have a simple tool and we know how much the community is tied to coronary angiography. We have some two-dimensional enhancements, but today this new tool is bringing 3D visualization and showing the stent from a different perspective. It’s making the expansion of the stent longitudinally available but also has the capability to go cross section by cross section and take accurate measurements.
How much clinical information can you get from 3DStent reconstruction?
Dr. Benamer : I am a big user of 2D stent expansion visualization tools (StentViz) and that is very useful, but I always felt limited by the information provided. So, I always dreamed about a 3D angiography tool, and GE did it.
Dr. Collet : For the first time, we have a detailed description of the stent during the procedure without the use of intracoronary imaging which will facilitate the assessment of the expansion. We’re quantifying the information we receive from 3DStent and are starting to understand that this technology is also able to provide us, using angiography alone, measures of Minimal Stent Area.
Dr. Guagliumi : With 3DStent, you can see the longitudinal view and then we can see inside the stent. So, you can see not only the longitudinal arrangement and expansion of the stent but also the cross-sectional area from the inside.
What advantages do you see with this new technology and what potential does it have?
Dr. Benamer : We clearly see from 3DStent additional information about the prosthetic and its correct deployment. For example, in the case below (), rotating the volume and playing with the slices will bring additional information compared with the initial view. We see that the rotation () shows the expansion of the stent but also one possible explanation with what we think to be calcium impeding the correct stent expansion.
Dr. Collet : I see 3DStent actually bridging the gap resulting from the lack of use of intravascular imaging in a systematic way in most of our Cath labs. It will provide the physician with the information they need to actually perform an optimal procedure. It’s intuitive to analyze and it literally takes 10 seconds to understand what we’re seeing during the live procedure. It’s a game changer. This technology has the potential to help us understand where the stent has been actually placed and if it has resulted in under expansion, we can fix it with additional maneuvers such as post-dilatation.
Dr. Guagliumi : By providing more information in a simple way, 3DStent has the potential to improve daily practice of interventional cardiologists.
3DStent solution includes Allia™ system, 3DXR and Volume Viewer Innova and requires AW workstation with Volume Viewer. These applications are sold separately. Available on Allia™ IGS 5 with 20cm or 30cm detector and Allia™ IGS 7 with 30cm detector. Commercial availability of GE HealthCare medical systems is subject to meeting local requirements in a given country or region. Contact a GE HealthCare Representative for more information. Intended for healthcare professionals only. The statements described here are based on their own opinion and on results that were achieved in their unique setting. Results may vary. JB26610XX