Dr. Försth, can you describe the activity of your hospital?
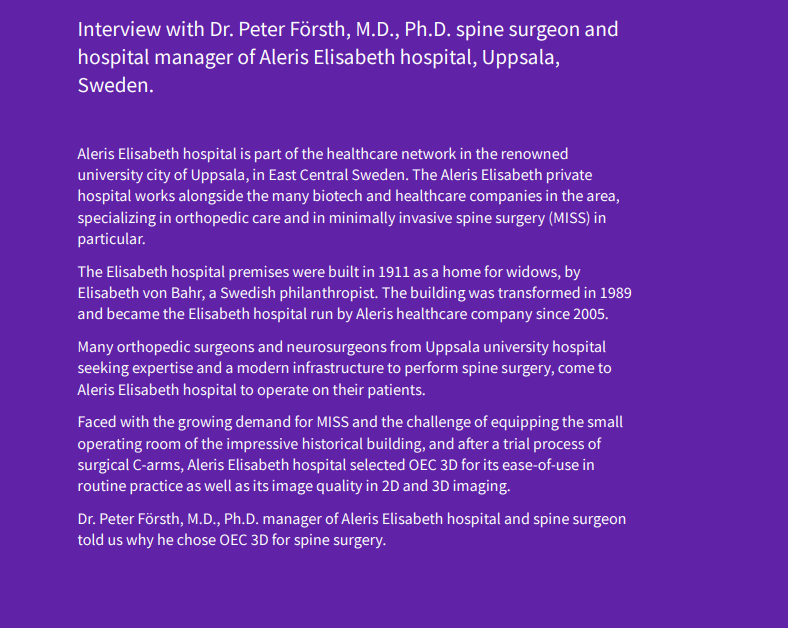
‘Aleris Elisabeth hospital is a private general orthopedic hospital treating musculoskeletal disorders of the shoulder, hand, hip, knee and spine. Spine surgery represents about one-third of the total volume of our surgical procedures. In this hospital, we also have the mission to train university medical students in our areas of expertise. I myself teach young specialists in spine surgery and I’m engaged organizing classes for spine surgeons of the Swedish Society of Spine Surgery. Some of these surgeons working at Uppsala university hospital bring their patients in our hospital to perform the surgery with our facility and staff. About 80% of the spine surgeries done in Aleris Elisabeth hospital are performed by surgeons from Uppsala university hospital. Beside my clinical work, as the manager of Aleris Elisabeth hospital, I am also in charge of organizing the entire orthopedic surgery activity. The orthopedic hospital accommodates 16 beds. We treat patients coming from the region of Uppsala, and also from other regions in Sweden. Surgery is performed in three operating rooms (OR) with three C-arms. The OR staff is trained to perform all types of orthopedic surgical procedures and rotates in the three ORs. One anesthesiologist supervises the anesthesiology nurses. As we have spine surgery almost every day, we dedicated OEC 3D to the spine surgeons who are assisted by at least one scrub nurse, one anesthesiology nurse, and one circulating nurse.’
How does OEC 3D contribute to supporting your surgical activity?
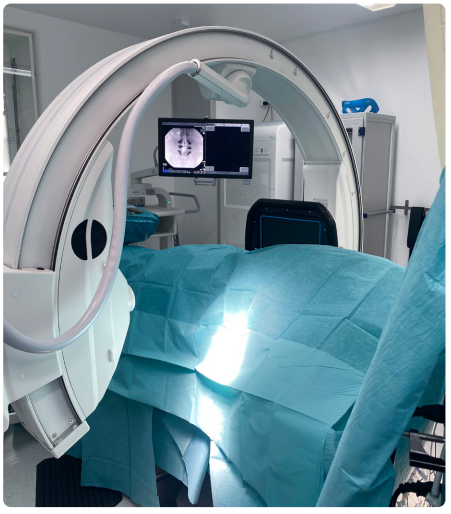
‘The OEC 3D C-arm that we acquired one year ago is mainly being used for spine surgery. The staff assists surgeons in operating the OEC 3D C-arm during the surgery. Surgeons use the workstation menu of OEC 3D to review the 3D images.
“One real advantage of OEC 3D is that it is a pretty user-friendly 3D C-arm.” Dr. Peter Försth
The instructions on the screen for the user operating the C-arm are very clear.
During my career, I have worked with other mobile 3D imaging and navigation systems that were more complicated to use.
With OEC 3D, we already know that the imaging part is quite easy. Indeed, we use 2D imaging for all our procedures and we use 3D imaging for lumbar fusion procedures, which represent approximatively 80 to 90 procedures per year.
After lumbar fusion, the most common procedure is lumbar decompressions followed by lumbar disk herniations that we treat with a minimally invasive approach using 2D imaging. We also perform anterior cervical discectomy and fusion (ACDF) and posterior cervical surgery with 2D and 3D imaging.
We are developing our treatment offering for MISS through the use of endoscopic surgical techniques. Endoscopic spine surgery is a hot topic. This is a very interesting surgical technique for which we need 2D imaging to place the endoscope and its tools correctly in the patient.
“With OEC 3D we obtain a good image quality: it’s quite easy to find the anatomical structures you need when you do endoscopic surgery.”
Dr. Peter Försth
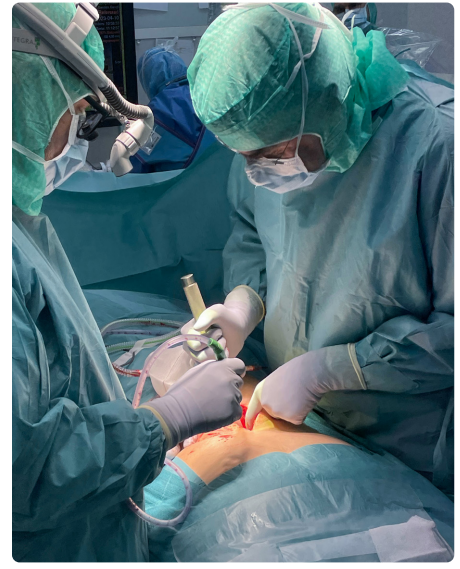
As I mentioned earlier, we always perform a 3D scan as a postoperative check before closing the wound in lumbar fusions. Some of our orthopedic surgeons are also interested in performing a 3D scan during osteotomies of the knee. Currently, orthopedic surgeons have used OEC 3D, but only for 2D imaging, and have found it to be very useful due to its large field of view. They are considering doing 3D scans however they don’t have access to OEC 3D that we are using almost every day for spine surgery. The space in our OR is quite small, so the 3D C-arm couldn’t be a bulky system. We selected OEC 3D after testing different C-arms because it’s a user-friendly and compact C-arm. When testing for the selection, it was also important for us to get a feeling of how OEC 3D would fit into our daily practice. We trusted GE HealthCare’s ability to provide us with application and service logistical support. This was another criterion that played a role in our selection. OEC 3D represents a significant investment for our hospital.
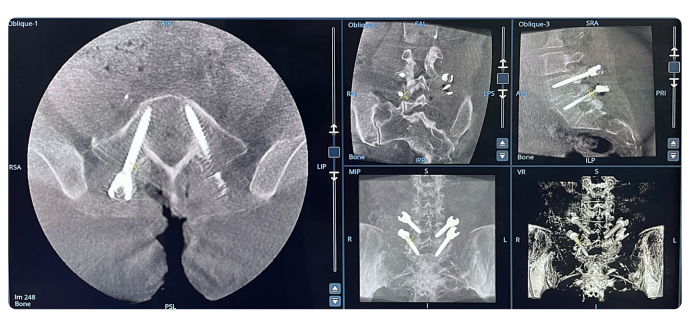
As a surgeon and the manager of the hospital, the most important thing for me is patient safety: before we close the wound, when we have finished with our surgery, we want to be able to verify that the implants are in the proper position. With OEC 3D in the OR, we do a final CBCT of the implants and get an assessment directly.
By investing in perioperative 3D imaging, surgeons can revise implant’s malplacements if needed before finishing the surgery. We are assured of providing a better patient care experience and we reduce the risk of revision surgeries and their associated costs and discomfort for the patient.
Of course, it is also an economic benefit for the hospital to eliminate the need of postoperative CT exam. This is particularly true of our hospital given that we don’t have the capacity to do CT imaging in our facility and had to send our patients to the university hospital. It’s quite demanding and delays the assessment of the screw placement after the surgery. It is not a very good quality of care.
Before working with OEC 3D, we used radiographical images for postoperative control, but this procedure is not accurate to estimate the screw placement in the body. We don’t do it anymore. It saves time and cost, but as I told you, the most important win is patient safety.
“The perioperative CBCT images from OEC 3D are of a much higher quality than the postoperative imaging diagnostic with which we were working.”
Dr. Peter Försth
What OEC 3D features do you use most for 2D imaging? ‘The OEC 3D C-arm gives an excellent image quality in 2D imaging. Working with a motorized C-arm was a new experience for us, and initially, we thought it would be difficult. That is not the case at all. Surgeons, who had to move the C-arm themselves as they wished, can rely on the staff to operate the equipment. The joystick is easy to handle and is used when the surgeon needs small changes in the angles. The staff also learned how to move the C-arm from AP views to lateral views, or for other larger angles, by setting and using the preset memory buttons. It is therefore easy to access the body part that we want to image. Another important benefit of OEC 3D is that the image covers a larger part of the spine. With our previous C-arm, the anatomical coverage was smaller. We configured OEC 3D with our application referent, so that it automatically starts with the preferred parameters: spine imaging profile, standard fluoroscopy, and low dose mode. For very obese patients as well, I feel that we don’t have to adjust anything. OEC 3D also gives us good imaging for these patients. We also use the Live Zoom especially when inserting pedicle screws and we want to magnify certain parts of the anatomy.’ How do you set up OEC 3D to perform the 3D scans? ‘For the 3D scan, we set the Standard mode or High Definition mode. We also use the metal artifact reduction (MAR) filter to verify the position of the implants in the volumetric images.
“With this OEC 3D configuration, we don’t have metal artifacts, and we see what we need to see i.e.”
Dr. Peter Försth
With this OEC 3D configuration, we don’t have metal artifacts, and we see what we need to see i.e., we see the cortical bone of the vertebra, and we see the metal in the screws. We also clearly see the borders of the vertebra. I review the volumetric images on the OEC 3D workstation myself. I look at the sagittal and also the axial views in general. I don’t use volume rendering (VR) as much. VR is a very nice illustration of what we have done, but clinically it is not completely relevant to verify the screws placement. The size of the 3D volume that we get with OEC 3D is quite enough for the type of fusion surgeries we perform. We don’t operate on large deformities, so the anatomy we see today in the 3D volume is more than sufficient and of very good quality. When doing the 3D scan, everyone stays inside the room. Of course, we move away from the C-arm and the sterile staff goes behind a leaded screen. As we all wear a lead apron, we just need to move away from the C-arm to protect ourselves from X-ray radiation. Over time, we have learned to better set up the patient and the table accessories for the 3D scan. It was quite easy for the staff to learn how to use OEC 3D. We receive no protests during application training! The staff also see the benefits for the patient when they look at the 3D images and can assess whether the implants are correctly placed. We have good feedback on OEC 3D from all the operating room staff."
How do you foresee your activity evolving with OEC 3D?
'With OEC 3D, we plan to develop endoscopic spine surgery as well as intraoperative spine navigation to manage X-ray radiation even more during some spine surgery procedures. The Swedish healthcare system is an evidence-based medicine and recommends continuing the placement of pedicle screws without robotic support. We plan to continue working with the free-hand technique and with perioperative 3D imaging. We are also working to have all the images entered in the university hospital PACS system so that we can share all our images from OEC 3D.’
“OEC 3D really brings clear benefit for the patient in terms of patient safety, but also for the surgeon as you can be sure of your surgery before you close the wound.” Dr. Peter Försth