New information regarding COVID-19 continues to emerge daily. This content was based on the sources available at the time of writing. Acute Cardiac Complications of COVID-19: What We Know Now contains more updated information regarding COVID-19's effect on the heart.
As empirical and anecdotal evidence feeds in about COVID-19, cardiologists have directed attention toward potential cardiac complications that the viral disease has been known to cause, particularly among patients with underlying heart conditions.
Given insights that indicate comorbidities both increase infection risk and worsen prognoses, physicians should remain diligent about patients' risk and refer them for imaging follow-ups to detect abnormalities. As an essential tool for monitoring heart activity, ECG may be a first line of defense in spotting signs of complications.
Cardiac Complications of COVID-19
Data from Wuhan, China has indicated that arrhythmia and acute cardiac injury could be among the most prevalent heart complications in confirmed-positive cases. A February 2020 case report in the Journal of the American Medical Association (JAMA) identified those complications in 16.7% and 7.2% of hospitalized patients, respectively.1
According to the American College of Cardiology (ACC) COVID-19 Clinical Guidance, other patients have presented with myocardial infarction, myocarditis, acute-onset heart failure, and cardiac arrest, which comport with two previous coronavirus outbreaks: severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS).2
Disease-triggered cardiometabolic demand and associated complications can worsen prognoses for patients with underlying heart conditions, especially those with cardiovascular disease (CVD). The overall case fatality rate for COVID-19 patients has stayed relatively stable at 2.3%, while individuals with CVD face more than quadruple the risk at 10.5%. CVD patients also face a higher risk of getting infected with the novel coronavirus. So far, little is known about cardiac complications in COVID-19 patients who don't have underlying heart conditions.
As evidence mounts about the severity of COVID-19 in vulnerable populations, the ACC recommends diligence and caution, adding that practitioners should monitor patients for potential cardiac complications as a result of the virus and refer to echocardiography.
Below are some key indicators that may present in ECG analysis, as well as potential signs to watch for in hospitalized patients.
How Complications May Present on ECG
While ECG presentations vary, TCTMD has reported that cardiologists should be aware of any symptoms indicative of impending cardiac events, especially in tandem with other clinical indicators such as elevated troponin or lab work that could suggest acute inflammatory response, including high levels of C-reactive protein, interleukin-6, CD4, and CD8.3 As these developments emerge, they may warrant an ECG.
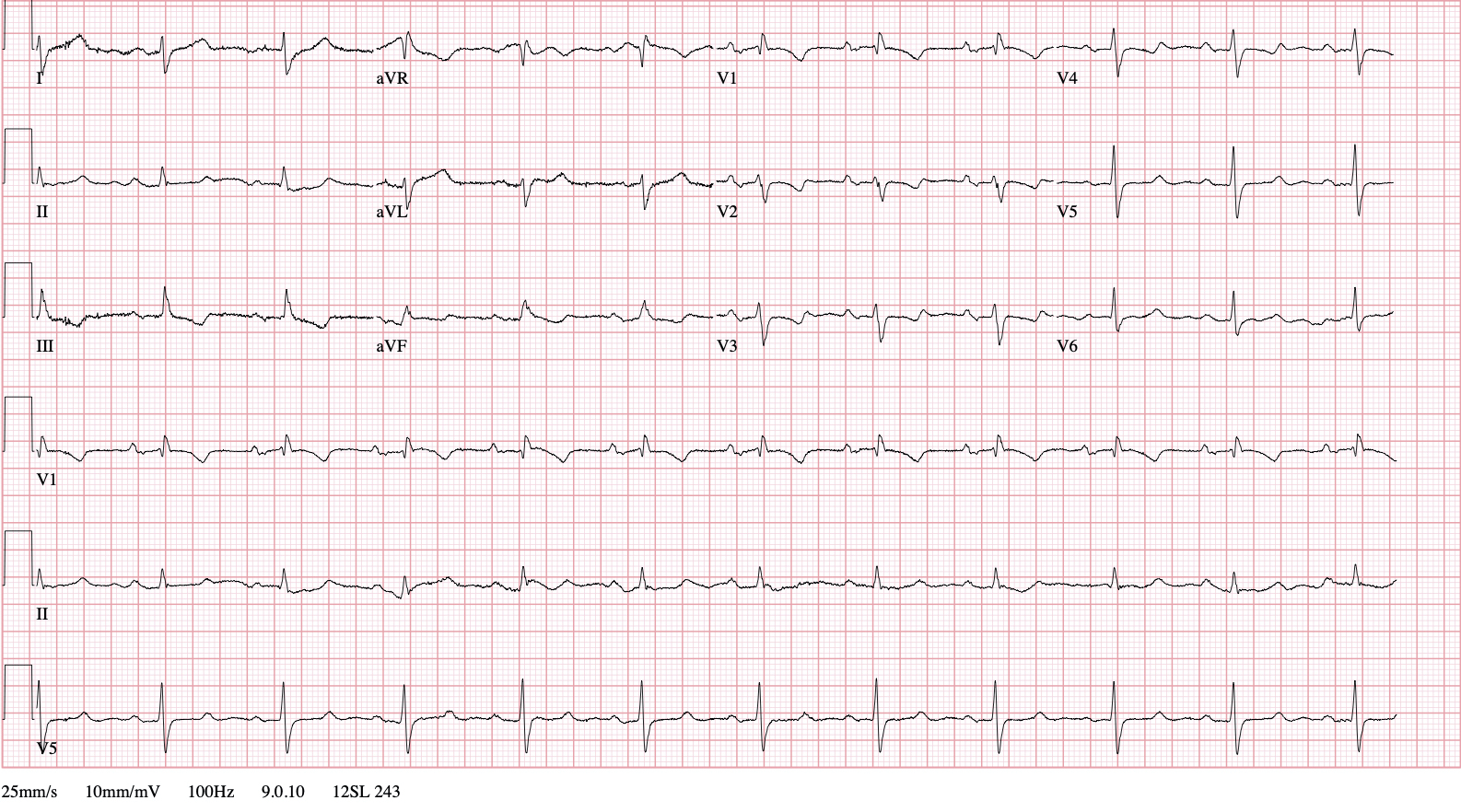
This ECG exhibits right axis deviation, right bundle brand block, S1Q3T3 and T-wave inversion in leads V1-V4 —
all finding consistent with right heart strain.
Generally, signs of complications may present on ECG in the following ways:
Arrhythmia
Arrhythmias manifest variably on ECG dependent on the rhythm disorder, but it may be important to watch for signs of A-fib. In one early study preprinted in medRxiv, some critical COVID-19 patients developed newly-onset A-fib, prompting the need to watch for these signs to preempt mortality:4
- Heart Rate: 350 to 650 beats per minute (A); slow-to-rapid (V); can be too low or too high depending upon ventricular response to chaotic atrial arrhythmia
- Rhythm: Irregular
- P Wave: Absent fibrillatory (F) waves
- QRS: <0.12 seconds
Acute Cardiac Injury
In one JAMA study that investigated cardiac injury among COVID-19 patients, all ECGs taken during biomarker elevation indicated abnormal heart activity, with researchers adding that the presentations aligned with myocardial ischemia.5 Notably, cardiologists may want to look for depression of the ST segment, depression and inversion of the T wave, and Q waves. The study provided a supplement of ECG graphs from three patients (ages 73, 47, and 76) who demonstrated these changes.6
Myocarditis
One expert suggested to TCTMD that inflammatory response as a result of the viral infection could lead to multiorgan damage, which may spell bigger problems than myocarditis alone. Still, cardiologists will want to monitor for potential changes, such as abnormalities in the T wave and ST segment. Additionally, sinus tachycardia and conduction defects (such as right- and left-bundle branch blocks and atrioventricular blocks) may also indicate myocarditis. These conditions are evidenced by the following:
- Sinus Tachycardia: Indicators include a heart rate over 100 beats per minute, regular rhythm, identical P waves before each QRS, PR intervals between 0.12 and 0.20 seconds, and QRS under 0.12 seconds.
- Conduction Defects: Presentations vary depending on the specific defect. Branch blocks, for example, have identical P waves before each QRS, PR intervals between 0.12 and 0.20 seconds, QRS of 0.12 seconds or less, and unique characteristics, such as ST elevation or RSR' in V1.
Cardiac Arrest
Though research assessing the predictive value of ECG for sudden cardiac arrest is limited, previous studies have provided some insights. For example, one paper in the International Journal of Heart Rhythm discussed ECG presentations that could identify risk, including pathologic Q waves (as with prior scar tissue or myocardial infarction) and RSR' patterns.7
Myocardial Infarction (MI)
Because COVID-19 shares some symptoms with heart attack, the ACC has cautioned about the possibility of MI going undiagnosed. Providers would do well to review essential patterns indicative of MI, including—as Healio outlines in a series of illustrative graphs—anterior/inferior/posterior STEMI and STEMI with right- and left-bundle branch blocks.8
Remember the Limitations of the Ongoing Situation
Given its newness and changing nature, the pandemic presents scientific limitations. As the science continues to develop and international practitioners share their findings and experiences, the data will undoubtedly change—as will recommendations for managing cardiac complications of COVID-19.
While this new evidence unfolds, cardiac monitoring will continue to play a key role in treatment planning. Be diligent, watch for changes in ECG, refer to advanced imaging when it is needed, and stay on high alert for abnormalities that could indicate problems.
References:
- Wang D, Hu B, Chang H, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. Journal of the American Medical Association. Feb. 2020; 323(11): 1061-1069. https://jamanetwork.com/journals/jama/fullarticle/2761044
- American College of Cardiology Clinical Bulletin. COVID-19 clinical guidance for the cardiovascular care team. American College of Cardiology. https://www.acc.org/~/media/Non-Clinical/Files-PDFs-Excel-MS-Word-etc/2020/02/S20028-ACC-Clinical-Bulletin-Coronavirus.pdf Accessed Jan. 24, 2022.
- Wood S. COVID-19 and the heart: Insights from the front lines. TCTMD. https://www.tctmd.com/news/covid-19-and-heart-insights-front-lines Accessed Jan. 24, 2022.
- Hui H, Zhang Y, Yang X, et al. Clinical and radiographic features of cardiac injury in patients with 2019 novel coronavirus pneumonia. MedRxiv. Feb 2020. https://www.medrxiv.org/content/10.1101/2020.02.24.20027052v1.full-text
- Shaobo S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. Journal of the American Medical Association. March 2020; 5(7): 802-810. https://jamanetwork.com/journals/jamacardiology/fullarticle/2763524
- Shaobo S, Qin M, Shen B, et al. Supplemental online content: Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. Journal of the American Medical Association. March 2020. https://cdn.jamanetwork.com/ama/content_public/journal/cardiology/0/hoi200024supp1_prod.pdf?Expires=2147483647&Signature=4sZ3ZrMgl9KrL0VHiGPtll8TJMfsHkMYPUl-FQ0eghV0eQuibQwOdbRx~OhWkjPoFwYLl62QboKocFEcVOFjFyk0SOuO5EBqMf2XFwxCyZJM9SzmUAD76JGDYhtxj5DPVn-3ek-7UJEWraUjj4zeJE~xW4IX2azTiHm2F4em61Zq86NLimahPGzl71eBNydLP1z78uFoPiCPsgjaSsSaJ9p2tb5lt3-SGqQv2CpsFYfI~Fusv~bu60spsQVjus6UbK-q5v5wr5Kixj7CMNsFZznUxfZh16PI-vlzCs7A0WxxvVB9m7S2YCreWQcmbygVe5P5hZ9JrIJ6TKckiMEsTQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA
- Chang C, Minglong C. Electrocardiography clues of sudden cardiac death: From close look to deep learning. International Journal of the Heart Rhythm. Feb 2019; 3(2): 39-40. https://www.ijhronline.org/article.asp?issn=2352-4197;year=2018;volume=3;issue=2;spage=39;epage=40;aulast=Cui
- Lome S. Top 5 MI ECG patterns you must know. Healio Learn from the Heart. https://www.healio.com/cardiology/learn-the-heart/ecg-review/ecg-interpretation-tutorial/stemi-mi-ecg-pattern Accessed Jan. 24, 2020